Hemorrhoids are swollen blood vessels that form in and around the rectum. After formation, they can cause symptoms such as itching, pain and bleeding, causing hemorrhoid sufferers to seek timely relief. Many assume that the best way to find relief is to shrink their hemorrhoids. And that’s why we often hear the question, “Does Witch Hazel Shrink Hemorrhoids Fast?”
In this post, we explain how witch hazel can be used for hemorrhoids and what results you can expect from this product. We also highlight ways to quickly shrink symptomatic hemorrhoids without undergoing surgery.

What is Witch Hazel?
This is a type of plant with reported medicinal properties. Over the years, extracts from the plant have been used to treat everything from acne and alopecia to eczema and psoriasis. Witch hazel extracts are also commonly found in over-the-counter relief products such as cream for hemorrhoids.
How Does Witch Hazel Affect Hemorrhoids?
When hemorrhoids symptoms are causing considerable discomfort, we know you’d like fast relief. Now, witch hazel can provide temporary relief for hemorrhoid sufferers. However, that relief does not come from shrinking hemorrhoids. Instead, this plant extract acts as an astringent when applied to your rectal area, causing cells to temporarily contract. In turn, symptoms such as burning and itching should improve. Unfortunately, they are likely to return once the witch hazel application wears away.
What Does Shrink Hemorrhoids?
If you have grade 1 hemorrhoids, you may find sufficient relief from witch hazel applications in combination with lifestyle changes to reduce your risk for recurring problems. For lasting relief of grade 2-3 internal hemorrhoids, however, a medical procedure to shrink hemorrhoids is likely to be your best option. At the Texas Hemorrhoid institute, our internal radiologists perform HAE, (hemorrhoid artery embolization), a procedure that shrinks internal hemorrhoids by cutting off their blood supply. And, while the hemorrhoids shrink slowly following your procedure, they should not return in the same location. So, if you’re looking to witch hazel to shrink hemorrhoids fast, we encourage you instead to instead request a consultation request a consultation request a consultation with our team and start exploring more effective treatment options.
Sitting on the toilet for too long can take a major toll on your health. But why is that the case? Here's what you need to know.

Sitting on the Toilet for Too Long: What's the Problem?
While there’s no specific period of time that’s safe or unsafe when you’re hanging out in the bathroom, experts suggest spending no more than 10-15 minutes doing your business to reduce your hemorrhoid risk. Ideally, however, you’d avoid distractions like scrolling on your phone, since it can lead to a condition known as ‘TikTok tush. In fact, a recent study published in the journal PLOS One revealed that people who used their phones in the bathroom were 46% more likely to develop hemorrhoids. The researchers concluded that the risk increase resulted from distracted phone users sitting on the toilet for too long. To reduce the risk, they suggest, you should finish passing your bowel movement in five minutes or less. But why is that shorter time-frame so important?
When you sit on the toilet for an extended time-period, you compress some of the nerves in your perineum. (The portion of skin between the anus and scrotum for men, or the anus and vulva for women.) So, right off the bat, you may experience numbness in the area. And, your feet and legs could even start tingling once you stand up after finishing your business.
Moreover, when you're sitting too long on the toilet, you put a lot of pressure on your anus and rectum because remaining in this position causes blood to pool in your anal veins. That's true whenever you sit for too long, but perching on the toilet adds extra pressure to the area because the cut-out center of the seat allows the rectum to sit lower than your buttocks. And, with all that pressure, you're more likely to develop hemorrhoids
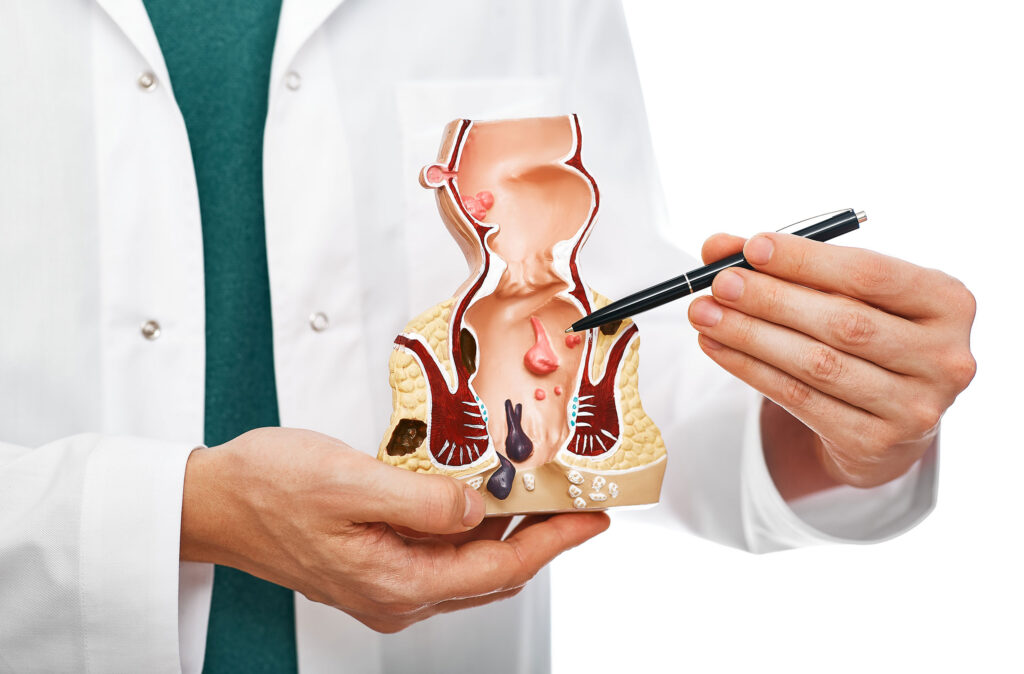
What are Hemorrhoids?
Hemorrhoids are simply veins in your rectum that become enlarged. But why does the pressure of sitting too long on the toilet increase your risk for these enlarged veins? Well, when you're sitting down, the force of gravity allows blood to pool in your rectal veins. That puts pressure on the veins, impeding blood flow and allowing them to bulge. Soon, you may experience symptoms such as pain, itching or bleeding when you pass a bowel movement. (That last symptom is associated with internal hemorrhoids, which form inside your rectum.) At that point, it's time to seek relief with hemorrhoid treatment.
Internal Hemorrhoid Relief in Houston and Dallas
Been sitting on the toilet too long and now you're experiencing unpleasant internal hemorrhoid symptoms? We're here to help! Click here to request an appointment Click here to request an appointment Click here to request an appointment with our interventional radiologists at the Texas Hemorrhoid Institute. When you come in, we'll review your minimally invasive treatment options!
Hemorrhoids are swollen blood vessels that form in our around your rectum and anal opening. They typically develop when that area of your body comes under excess pressure, and constipation could contribute to that pressure. For that reason, a diet that’s high in fiber can help reduce your risk, which is why we suggest eating these five foods to prevent hemorrhoids.

Fiber and Constipation
You can find fiber in several types of food sources, including nuts, seeds, grains, fruits and veggies. There are two types of fiber:
- Soluble, meaning it dissolves in water
- Insoluble, meaning it won’t dissolve in water
A healthy diet should contain a blend of both soluble and insoluble fiber. This mix helps prevent constipation by making stools both larger and softer. That way, they pass at a faster pace when moving through your body, and they are easier to pass when it’s time to head to the bathroom. This reduces the amount of time you spend on the toilet, and helps you avoid straining when you pass a bowel movement, both of which can be causes of hemorrhoids.
High-Fiber Foods to Prevent Hemorrhoids
Some people take fiber supplements for hemorrhoids. But you can actually add more fiber to your diet naturally with these five foods. As a bonus, they are packed with plenty of other nutrients and substances that your body needs to function optimally, so by choosing these foods to prevent hemorrhoids, you may also improve your general well-being. Just remember to increase your fluid intake when eating more fiber. An increase in fiber intake without adequate hydration can lead to constipation which of could cause worsening hemorrhoid flares and inflammation.
- Kiwis: this tasty choice is a great source of soluble fiber, with each fruit containing 2 grams. (The average daily goal is between 25 and 38 grams each day, though totals vary depending on your age, gender and current state of health.) Simply eating two kiwis a day for four weeks helped participants in this study increase their daily bowel movements and improve overall comfort with their digestive systems.
- Apples: containing both soluble and insoluble fiber (as long as you keep the skin on your fruit), this crunchy favorite will help keep you from sitting on the toilet for too long.
- Barley: Containing 6 grams of soluble fiber per cooked cup, this old-school grain can really soften stools to help make the go more comfortable. Try adding it to a soup or using it as a rice replacement in your favorite rice recipes.
- Lentils: Another soup staple, this is one of the best foods to prevent hemorrhoids because it’s both a great source of fibroid and it can help nourish the healthy microbes in your gut, supporting optimal digestion and better overall health.
- Popcorn: This choice may be surprising, but popcorn is packed with 1.2 grams of insoluble fiber per cup. Keep this food choice in the healthy realm by skipping the butter and salt, and you’ve got a fun and easy way to sneak more fiber into your daily diet.
Help for Existing Hemorrhoids
While fiber can help reduce your risk for hemorrhoids, dietary changes alone may not be able to resolve existing concerns. So, if you are dealing with grade 2-3 internal hemorrhoids, and want relief without surgery, we’re here to help. Contact the Texas Hemorrhoid Institute Contact the Texas Hemorrhoid Institute Contact the Texas Hemorrhoid Institute to learn more about minimally invasive treatment options.
Are piles and hemorrhoids the same thing? Yes, hemorrhoids is the medical term used to describe swollen veins located in and around the anus and rectum. Piles is an informal term used to describe the same condition. But how did they get these names? What symptoms do they cause and when should you seek treatment? Here’s what you need to know.

Are Piles and Hemorrhoids the Same?
These are two different names for the same condition. The word hemorrhoid has Greek and Latin origins that loosely translate to bleeding veins. Piles, on the other hand, is derived from the Latin word for ball, referencing the shape of a hemorrhoid. Both terms describe some of the common external and internal hemorrhoid symptoms, including:
- Swollen veins that bulge or protrude from the anal opening
- Itching
- Rectal Bleeding
- Leaking of mucus or even fecal matter
- Feeling full in the rectum
- Bowel discomfort
What is the Difference Between a Hemorrhoid and a Pile?
These two terms are used interchangeably, but there are two different types of hemorrhoids: internal and external piles.
Internal hemorrhoids form inside your rectum, and are graded on a severity level of 1 through 4 based on the degree of protrusion from the anus. They typically cause bleeding and itching. You can learn more about what stage of hemorrhoid you have here.
External hemorrhoids form beneath the skin surrounding your anus. They can be swollen, itchy and painful.
Some people have mixed hemorrhoids, meaning they develop both internally and externally, resulting in a combination of symptoms.
Do Piles Go Away On Their Own?
Mild hemorrhoids (stage 1) may self-resolve, especially with lifestyle changes that reduce your risk factors. (These include sitting less; softening your stool through dietary changes; avoiding straining when passing bowel movements; and getting regular exercise.) However, stage 2-4 internal hemorrhoids often require medical intervention. And, since stage 4 hemorrhoids typically require surgical treatment, many patients prefer seeking intervention before their piles progress to that point.
Want relief from the itching, bleeding and discomfort of stage 2-3 internal piles? The interventional radiologists at the Texas Hemorrhoid Institute perform HAE, or hemorrhoid artery embolization, a medical procedure that can treat internal hemorrhoids at these stages without the need for surgery. You can learn more and explore your HAE candidacy by requesting a consultation [/tx-appt-link.]
If you've been living with internal hemorrhoids, you may already be dealing with painful, disruptive symptoms. And that may be impacting several areas of your life. But if you're wondering, can you have intercourse with hemorrhoids, here's what you need to know.

What are hemorrhoids?
Hemorrhoids (or piles) are just enlarged veins in your rectum or anus. Sometimes, the walls of these vessels stretch very thin, causing bulging and irritation in the veins. Now, we classify internal hemorrhoids according to their degree of protrusion. You'll be diagnosed with:
- Grade 1 hemorrhoids
if they are small, and not visible or palpable. While unlikely to cause discomfort, they may cause bleeding when you pass a bowel movement. - Grade 2 hemorrhoids
are larger, and may pop out of the anus when you pass a bowel movement, returning on their own afterward. Symptoms can include pain, itching and bleeding. - Grade 3 hemorrhoids
are internal vessels that bulge outside your anal canal, and will not return unless you reposition them manually. They are also symptomatic. - Grade 4 hemorrhoids
are the most severe. The bulging vessels will stay outside the anal canal, even if you manually reposition them, and your symptoms are likely to be severe.
Can you have intercourse with hemorrhoids?
With more severe hemorrhoids, intercourse (either vaginal or anal) may be painful. (Note that anal intercourse can contribute to hemorrhoids, as was the case for Bravo TV star Scheana Shay.) Now, while this may prevent you from experiencing penetration, that doesn't mean you'll have to avoid intimacy altogether. Instead, you and your partner may need to find other ways to express your intimate connection. Then, once you relieve your discomfort with hemorrhoid treatment, you can return to your former sexual connections, following your recovery period.
Hemorrhoid Treatment in Texas
Here at the Texas Hemorrhoid Institute, we treat grade two and three internal hemorrhoids with Hemorrhoid Artery Embolization (HAE), a non-surgical procedure that relieves your symptoms with a fast recovery, reduced risk for side effects and minimal discomfort.
Wondering if you can have intercourse with hemorrhoids despite your pain, itching and bleeding? You may be able to connect with penetration without treatment. But you're more likely to enjoy intercourse and the rest of your daily activities after seeking treatment. Ready to begin your recovery journey? Click here to request an appointment Click here to request an appointment Click here to request an appointment with our hemorrhoid experts in Texas.
At the Texas Hemorrhoid Institute, we provide minimally invasive treatments for Grade 2-3 internal hemorrhoids. But how do you know what stage your hemorrhoid is at, in order to determine your best treatment options? In this post, we break down the hemorrhoid grading system to help you understand your treatment options.
How Do You Know What Stage Your Hemorrhoid Is?
Internal hemorrhoids are classified on a grading system of 1 – 4, based on their level of prolapse from the anus.
- Grade 1 Hemorrhoids: These swollen vessels may protrude into your anal canal, but they will not prolapse out of your anus.
- Grade 2 Hemorrhoids: Hemorrhoids will prolapse when you strain or pass a bowel movement, but they will return into your anal canal without assistance.
- Grade 3 Hemorrhoids: Protrusion occurs with straining or when passing a bowel movement, but return only happens with manual repositioning.
- Grade 4 Hemorrhoids: The hemorrhoid remains prolapsed outside of the anus.
Can Hemorrhoids Go Away On Their Own?
Grade 1 hemorrhoids may resolve without treatment, especially if you follow a diet to help hemorrhoids or make other lifestyle modifications. Grade 2 hemorrhoids may shrink without a medical procedure, but Grade 3 hemorrhoids will not self-resolve and Grade 4 hemorrhoids must be treated surgically. As such, it’s important to speak to your doctor as soon as you notice symptoms such as itching, prolapsing or bleeding when you pass a bowel movement. When you receive a diagnosis at an earlier grade of prolapse, you will be able to find relief with less invasive treatment options.
How Do You Know What Stage Your Hemorrhoid is in Need of Treatment?
While rarely dangerous, untreated hemorrhoids can cause intrusive symptoms that interfere with your quality of life. For that reason, seeking early treatment is the best way to prevent progression and protect your health. Ready to find relief from bulging, itchy and uncomfortable hemorrhoids? We’re here to help. [Tx-appt-link] Reach out to our team [/tx-appt-link] to request a consultation at one of our seven Texas Hemorrhoid Institute locations.
Hemorrhoids are merely swollen, inflamed vessels that form in and around the anal opening. However, certain hemorrhoid symptoms are similar to the symptoms of anal cancer and other diseases or conditions such as diverticulitis. As such, some people may conflate the side effects of hemorrhoids with cancer. But there are simple ways to detect the differences, and this post will help lead you to specialists, such as Hemorrhoid Doctors in Texas, who can give you a proper diagnosis.

Symptoms of Hemorrhoids
Hemorrhoids can form externally, meaning outside of the anus, causing itching, swelling and discomfort. And, when they form internally, they may not be painful but hemorrhoid symptoms there may include rectal bleeding, the leakage of mucus, itching or even protrusion.
Symptoms of Diverticulitis
Diverticulitis is a condition describing an infection of your diverticula (these are small pouches found in the lining of your colon.) Symptoms include abdominal pain and distension, fever, and changes in bowel habits; some of these overlap with symptoms of colorectal or anal cancer.
Symptoms of Anal Cancer
Again, while hemorrhoids aren’t a sign of cancer, the two conditions share common symptoms. In fact, according to the American Cancer Society, symptoms of anal cancer include bleeding from the anus, abnormal discharge from the anus and itching around the rectum, all symptoms that are also associated with hemorrhoids. However, unlike hemorrhoids, anal cancer can also cause:
- A lump or mass to form at the opening of your anus
- A feeling of pain or fullness in your anal region
- Changes to your bowel movements
- Loss of control over your bowels
- Swelling of the lymph nodes in your anus or groin
Hemorrhoids & Cancer: When to See a Doctor
Mild hemorrhoid symptoms may be resolved with homecare and lifestyle changes, including increasing your fluid and fiber intake to reduce constipation, making it easier to pass bowel movements and reducing pressure on your anus and rectum. At the same time, you should avoid sitting on the toilet for too long, or straining to pass a bowel movement. And, even if your stools are loose, try to address diarrhea as frequently passing stool can also irritate your anal region and contribute to hemorrhoid development.
However, if your symptoms persist or worsen, or if you experience any rectal bleeding, you should see a doctor right away. When you see a healthcare professional, you can distinguish hemorrhoids and cancer symptoms. Then, if internal hemorrhoids are to blame for your discomfort, you can request a consultation request a consultation request a consultation with the Texas Hemorrhoid Institute to discuss your treatment options.
Hemorrhoids form when you put pressure on the veins in and around your rectum. That pressure could come from many different sources, but one common trigger is suffering from constipation, or straining to pass bowel movements. Now, changes in your diet can help soften stool, making it easier to empty your bowels and reducing strain on your rectum. But should you take fiber supplements for hemorrhoids? Here’s what you need to know.

Do Fiber Supplements Help with Hemorrhoids?
Taking an over-the-counter fiber supplement for hemorrhoids could help with prevention. Not only can fiber supplementation reduce your risk for constipation, this study shows that it can reduce your risk for hemorrhoid symptoms such as rectal bleeding by as much as 50%. However, when supplementing fiber, it’s very important to maintain sufficient fluid intake. Otherwise, the supplements may not offer sufficient benefits.
What is the Best Supplement to Get Rid of Hemorrhoids?
An over-the-counter supplement like Metamucil (made from psyllium husk fiber) is a great first choice. Unfortunately, some people will experience gas and bloating with this kind of fiber supplement for hemorrhoids. If that’s the case for you, try switching to a wheat dextrin supplement such as Benefiber to see if that’s easier on your digestive tract.
Can Metamucil Shrink Hemorrhoids?
While fiber supplements can help reduce your risk for hemorrhoids, and may help you reduce your symptom burden, they ae unlikely to shrink severe hemorrhoids. (Remember, hemorrhoids are graded on four levels. So, while Grade 1 hemorrhoids may resolve with lifestyle changes such as dietary supplements and increased fiber intake, grade 2, 3 or 4 hemorrhoids are unlikely to shrink without medical intervention.
What Shrinks Hemorrhoids Fastest?
Even when fiber supplements for hemorrhoids can shrink these swollen veins, the process can take time. Plus, as we mentioned earlier, grade 2, 3 and 4 hemorrhoids may not shrink with supplementation. So, what’s a faster way to shrink your hemorrhoids and resolve symptoms such as itching and bleeding? If you want relief without surgery or overnight hospital stays, we invite you to contact the Texas Hemorrhoid Institute contact the Texas Hemorrhoid Institute contact the Texas Hemorrhoid Institute to learn more about HAE (hemorrhoid artery embolization.) This minimally invasive procedure is ideal for patients with internal grade 2-3 hemorrhoids, shrinking the veins by blocking their blood flow. When you come into the office, we can explore your candidacy and review all your treatment options.
If you're living with hemorrhoids, changing your diet could help. After all, spending too long on the toilet and straining to pass bowel movements are both risk factors for these swollen rectal veins, so changing the way you eat may speed things up in the bathroom, helping you feel better. So, what's the best diet to help hemorrhoids? Keep reading to find out.

Following a High Fiber Diet to Help Hemorrhoids
If you have hemorrhoids, following a high-fiber diet may help you manage your symptoms by allowing for softer stool that's easier for you to pass. If you have hemorrhoids, following a high-fiber diet may help you manage your symptoms by allowing for softer stool that's easier for you to pass. According to the Dietary Guidelines for Americans, 2020–2025, that means getting 14 grams of fiber for every 1,000 calories you consume. So, if you’re on a 2,000-calorie diet, you should aim to eat at least 28 grams of fiber per day. Here are some of the best foods to include in your meals:
- Whole grains, including bran and shredded wheat
- Fruits such as pears, apples, prunes and raspberries
- Veggies, especially green peas, collard greens, sweet potatoes and winter squash
- Navy, pinto and/or kidney beans
Additionally, increasing your daily water intake and engaging in regular exercise can help prevent or relieve hemorrhoid symptoms.
Foods to Avoid with Hemorrhoids
While adding high-fiber foods to your diet can help soften stools and ease hemorrhoid symptoms, reducing or eliminating these foods can further reduce your constipation risks.
Low-fiber foods to avoid:
- cheese
- potato chips
- fast and processed foods
- ice cream
- red meat
- frozen meals
When to Seek Further Intervention
For people with mild to moderate hemorrhoids, simple lifestyle changes may provide sufficient symptom relief. However, people with stage two or three internal hemorrhoids experience itching, discomfort, or bleeding with bowel movements. And so, to find lasting relief, you're likely to need additional medical support from Hemorrhoid Doctors in Texas.
Luckily, when a diet to help hemorrhoids isn't working, the experts at the Texas Hemorrhoid Institute are ready to dive in! Our interventional radiologists perform a procedure known as HAE, or hemorrhoid artery embolization. This minimally-invasive treatment option provides relief by reducing blood flow to your hemorrhoids. Shortly after, they shrink and disappear. And so do your symptoms!
In contrast to surgical treatment options, patients who choose HAE experience fewer complications and a shorter recovery period. Ready to see if HAE is the right treatment for you? Click here to request an appointmentClick here to request an appointmentClick here to request an appointment
When it comes to your health, seeing blood in the toilet after passing a bowel movement can be very concerning. In some cases, this could be a symptom of internal hemorrhoids, also known as piles. But in other cases, rectal bleeding could be a sign of cancer. In fact, while this 36-year-old marathon runner dismissed blood in his stool as a sign of hemorrhoids, he actually had stage 2 colorectal cancer! As such, determining the cause of blood in the toilet could be critical to your long-term health. This post will help you determine whether your rectal bleeding is caused by hemorrhoids or cancer.

Blood in Toilet: Color Matters
When you notice blood in the toilet when wiping or after passing a bowel movement, taking careful note of the coloring could help determine the cause of this symptom. As this viral TikTok video recently helped clarify, the color of the blood could help you determine the cause of the bleeding.
If your rectal bleeding is the result of hemorrhoids symptoms, the blood will be bright red in color, much like pizza sauce fresh out of the jar. In contrast, blood related to colorectal cancer may be darker in color.
In addition to rectal bleeding, both hemorrhoids and anal or colorectal cancer can cause protrusions in the anus, as well as changes to your bowel habits. While closely monitoring the color of the blood you see in the toilet, the best way to get an accurate diagnosis is to see a trusted healthcare provider. After, you can begin seeking appropriate treatment.
Hemorrhoid Relief in Houston and Dallas
If internal hemorrhoids are determined to be the cause of blood in the toilet, topical products may help temporarily. However, once you have bleeding, your hemorrhoids are likely severe enough that only a medical procedure will provide lasting relief. In such cases, we encourage you to visit us at the Texas Hemorrhoid Institute by requesting a consultation [/tx-appt-link.] In one of our Houston or Dallas area offices, we can review minimally-invasive treatment options such as HAE (hemorrhoid artery embolization) to help you find symptom relief without undergoing invasive surgery.